Neuropsychiatric Symptoms: A Caregiver’s Guide

What are Neuropsychiatric Symptoms?
Neuropsychiatric Symptoms (NPS) are the non-cognitive, behavioral manifestations of dementia. Just as those living with Alzheimer’s and other forms of dementia may develop a range of impairments that affect their capacity to remember, communicate effectively, and reason, they also may experience changes in mood and personality leading to troubling and disruptive behaviors. Although these behaviors – collectively referred to as NPS – contribute directly to caregiver stress and burnout, often they can be successfully addressed by working with professionals utilizing a variety of intervention approaches.

How Common Are NPS?
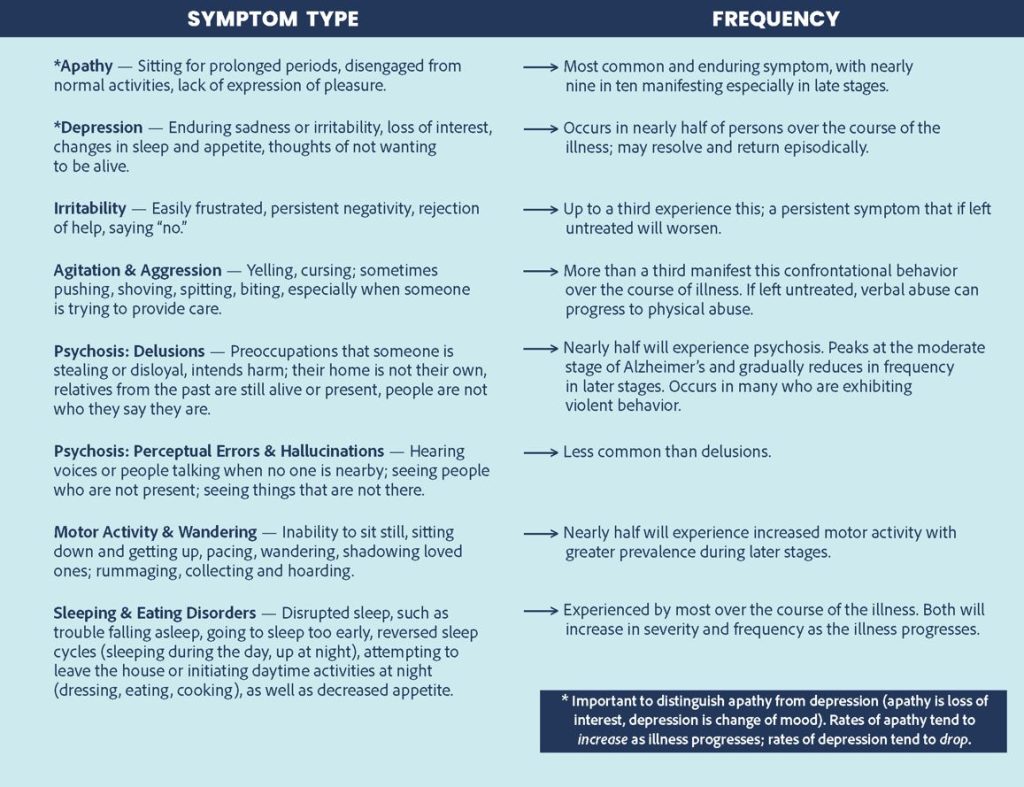
Studies show that nearly every person living with dementia will eventually develop some form of NPS. It is also important to be aware that behavioral symptoms – including apathy, depression, irritability, and psychosis – can be prodromes, symptoms that begin prior to the onset of memory impairment and other cognitive symptoms. They can be the first symptom of dementia.
Treatment Options
The first step in accessing an intervention is the engagement of a qualified dementia health care provider for a complete evaluation. This could be a geriatric medicine specialist, a neurologist, or a geriatric psychiatrist.
Non-Pharmacological Approaches
For mild cases, non-pharma approaches should be tried first: music therapy, aromatherapy, exercise or physical therapy, pet/animal therapy and, for some, psychotherapy. If these fail or if symptoms are persistent or severe, medications may be necessary.
Pharmacological Approaches
All medications carry risks that need to be discussed and weighed against possible benefits. Dementia-focused providers, especially geriatric psychiatrists, may recommend medications from the antidepressant class (selective serotonin reuptake inhibitors, SSRIs) or from the atypical antipsychotic class. Though often effective, use of antipsychotics is generally a last resort and should be approached with caution, as these have been associated with an increased risk of death. Use of sedative hypnotics should generally be avoided as they often worsen confusion and cause falls.
Clinical Trials
Experimental non-antipsychotic medication clinical trials are ongoing. Information about where these are offered and how to begin the process of enrollment can be found at clinicaltrials.gov.

Caregivers Need Care
Caregivers are often overwhelmed by a multiplicity of factors in attempting to provide the best quality of life for those afflicted with the cognitive and behavioral manifestations of dementia, leading to high rates of stress and depression that can result in a neglect of personal physical health and well-being. Help is available.
Seek support, guidance and resources by contacting the AFA Helpline, staffed by licensed social workers trained in dementia care, available 7 days a week via phone (866-232-8484), text (646-586-5283) or webchat by clicking the blue and white chat icon in the lower corner of the page.
Explore opportunities for respite care in your local community, spend time with friends, get outside for walks in nature, practice yoga or meditate, join a support group, or participate in psychotherapy. Remember, the physical and emotional demands of caring for a loved one with Alzheimer’s can be exhausting and lead to burnout. It’s important to maintain your own health and well-being.
Developed with the assistance of Jeremy Koppel, MD, AFA Medical, Scientific, & Memory Screening Advisory Board Member
Have questions or need more information? Contact AFA’s Helpline at 866-232-8484 or click the chat icon in the lower right hand corner of this page.


